Neuropathic Pain Treatment in Chesterfield
Relief for nerve-related pain caused by injury, compression, or chronic spine conditions—personalized care from Chesterfield’s leading spine specialist.

ADVANCED TECHNOLOGY MEETS
SURGICAL EXPERTISE
What Is Neuropathic Pain?
Neuropathic pain refers to pain that arises from damage to or dysfunction within the nervous system itself, rather than from muscles, joints, or other soft tissues. In neuropathic pain, nerves that normally transmit sensation become the source of pain signals, even when no active tissue injury is present. As a result, nerve-based pain often behaves differently from mechanical pain and tends to respond poorly to treatments aimed solely at muscles or joints.
Patients often describe neuropathic pain as burning, tingling, shooting, or electric in quality. Some experience pins-and-needles sensations, hypersensitivity to light touch, or pain triggered by temperature changes. Symptoms may persist at rest, worsen at night, or continue long after an initial injury has healed, which can make the condition difficult to understand and manage.
Neuropathic pain commonly develops after prolonged nerve compression in the spine, direct nerve injury, or structural changes that narrow the spaces around spinal nerves. Conditions such as spinal stenosis, herniated discs, and degenerative spine disease frequently contribute. Systemic conditions, including diabetes, may also damage peripheral nerves over time. Effective care depends on identifying the specific source of nerve dysfunction and tailoring treatment accordingly, rather than simply suppressing pain symptoms.
REDEFINING WHAT RECOVERY CAN LOOK LIKE
Common Causes of
Neuropathic Pain
Common Causes of
Neuropathic Pain
Common causes of neuropathic pain fall into a few broad categories, most involving compression, irritation, or direct injury to the nerves that carry signals between the spine, brain, and limbs.
Nerve Compression from Spinal Disorders
Conditions such as herniated discs, spinal stenosis (narrowing of the spinal canal), and degenerative disc disease may press on nearby nerve roots. Over time, sustained pressure disrupts normal nerve signaling and can cause burning, shooting, or electric pain that radiates into the arms or legs.
Nerve Damage After Surgery or Trauma
Spine surgery, joint surgery, or other procedures may irritate nerves, and scar tissue can form around nerve roots during healing. Major injuries, including falls, car accidents, or sports trauma, may stretch or bruise nerves, leading to persistent neuropathic pain even after the original injury improves.
Chronic Inflammation or Autoimmune Conditions
Long-standing inflammation in or around the spine may lower the threshold at which nerves generate pain. Autoimmune diseases, in which the immune system attacks the body’s own tissues, can damage nerves or their protective covering (myelin), resulting in ongoing pain and abnormal sensations.
Peripheral Neuropathy
Peripheral neuropathy involves damage to nerves outside the brain and spinal cord. Metabolic conditions such as diabetes, vitamin deficiencies, kidney disease, toxin exposure, and heavy alcohol use can injure these nerves over time, most often causing numbness, tingling, or burning pain in the feet and hands.
Other Contributing Factors
Infections such as shingles, repetitive strain on spinal or peripheral nerves, and untreated spine problems may allow nerve irritation to become chronic. Many patients have more than one contributing factor, such as mild spinal stenosis combined with diabetes, which makes thorough evaluation essential.



Recognizing the Symptoms of Neuropathic Pain
Neuropathic pain often presents with a distinct pattern of symptoms that differs from typical muscle or joint pain. Because nerve signals become distorted, symptoms may feel unpredictable, disproportionate to physical findings, or resistant to rest and activity modification.
Many patients report burning, tingling, stabbing, or electric sensations that affect the neck, back, arms, or legs. Pain may radiate along a specific nerve pathway, producing shooting discomfort similar to sciatica or cervical radiculopathy, and may travel well beyond the original site of injury. Numbness often accompanies pain, and some patients develop heightened sensitivity in which light touch, clothing, or temperature changes trigger significant discomfort.
Neuropathic pain can also interfere with strength, coordination, and balance, particularly when motor nerves are involved. Symptoms may persist at rest, disrupt sleep, or worsen at night, which contributes to fatigue and emotional strain over time. When nerve-related pain begins to limit daily activities, affect mood, or fail to improve with standard treatments, it often signals the need for a more targeted evaluation.
How Dr. Peloza
Diagnoses
Neuropathic Pain
Diagnosing neuropathic pain requires careful distinction between nerve-related symptoms and pain that arises from muscles, joints, or other soft tissues. John Peloza begins with a comprehensive clinical evaluation that includes a detailed medical history, a focused physical examination, and targeted neurological testing. This step helps clarify symptom patterns, identify nerve involvement, and rule out non-neurologic sources of pain.
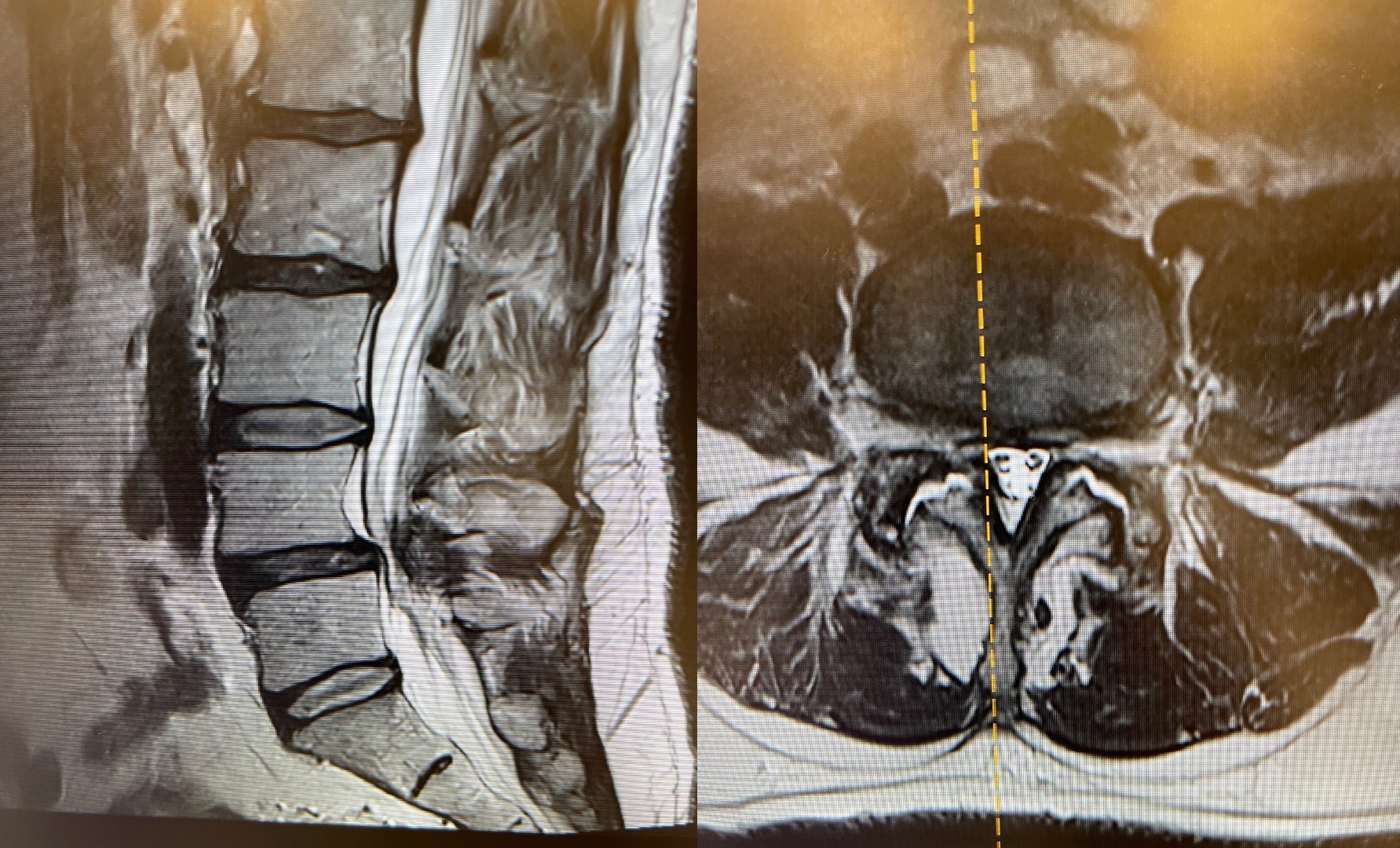
Advanced imaging plays a central role in this process. Magnetic resonance imaging or computed tomography allows precise assessment of the spine and surrounding structures, with particular attention to areas where nerves may face compression or irritation. These studies help identify conditions such as disc herniation, spinal stenosis, or degenerative changes that correlate with a patient’s symptoms rather than incidental findings alone.
When symptoms and imaging require further clarification, electrodiagnostic studies may be appropriate. Electromyography and nerve conduction studies assess the electrical activity of muscles and nerves, which can reveal impaired signal transmission and localize the level of nerve dysfunction. In select cases, diagnostic injections and pain mapping provide additional insight by temporarily numbing specific nerves to confirm their role in generating pain. Together, these tools allow Dr. Peloza to define the true source of neuropathic pain and guide treatment with precision rather than trial and error.

Non-Surgical
Treatment Options
Non-surgical treatments focus on calming irritated nerves, reducing inflammation, and improving how the spine and supporting muscles function.
- Medications: Targeted nerve medications such as gabapentin and pregabalin can help reduce burning, tingling, and shooting nerve pain by stabilizing overactive nerve signals. Anti-inflammatory medicines and, in some cases, muscle relaxants or topical creams may be added to ease surrounding inflammation and muscle tension.
- Physical Therapy: Structured physical therapy builds strength in the core and back muscles that support the spine, which can reduce pressure on irritated nerves. Gentle stretching, posture training, and movement retraining also improve flexibility and reduce flare-ups linked to everyday activities.
- Spine Injections: Epidural steroid injections or selective nerve root blocks deliver anti-inflammatory medication directly around compressed or irritated nerves. These injections can decrease pain signals, reduce swelling, and create a window of relief that allows patients to participate more fully in rehabilitation.
- Electrical Stimulation (TENS): Transcutaneous electrical nerve stimulation (TENS) uses low-voltage electrical currents applied through the skin to interrupt or “distract” abnormal pain signals traveling to the brain. Over time, regular use may help some patients experience less intense pain and improved function.
- Lifestyle & Nutritional Support: Addressing excess weight, systemic inflammation, and poor posture can lessen mechanical stress on the spine and nerves. Smoking cessation, ergonomic changes at work and home, and consistent low-impact exercise (like walking or swimming) support nerve health and long-term pain control.
Advanced and Minimally Invasive Procedures
- Endoscopic Decompression: Endoscopic decompression uses a tiny camera and specialized instruments through a small incision to remove small pieces of bone, disc, or thickened ligament that are pressing on spinal nerves. This approach aims to relieve nerve compression while minimizing muscle disruption, blood loss, and recovery time compared with traditional open surgery.
- Spinal Cord Stimulation (SCS): Spinal cord stimulation is typically reserved for select patients with chronic neuropathic pain that has not improved with other treatments. A small device delivers mild electrical impulses to the spinal cord, which can modify how pain signals are transmitted to the brain and, for some patients, reduce the intensity or unpleasantness of their pain.
- Artificial Disc Replacement (in select cases): Artificial disc replacement involves removing a damaged spinal disc that is compressing nerves and replacing it with a motion-preserving implant. Unlike spinal fusion, ADR is designed to maintain more natural movement at the treated level, which can reduce stress on nearby segments while still decompressing the affected nerves.
- Spinal fusion (in select cases): Permanently connects two or more vertebrae to stabilize unstable segments and protect spinal nerves when less invasive or motion-preserving options are not appropriate.


When Patients Should See a Specialist in Chesterfield for Neuropathic Pain
Neuropathic pain warrants evaluation by a spine specialist when symptoms persist, progress, or begin to interfere with safety, function, or quality of life. While some nerve irritation improves with time and conservative care, ongoing or worsening symptoms often signal a problem that requires more precise diagnosis.
You should consider seeing a specialist if burning, tingling, numbness, or shooting pain lasts more than a few weeks, particularly when it affects the arms, hands, legs, or feet. Pain that worsens with walking, standing, or lying down at night may reflect ongoing nerve compression that is unlikely to resolve on its own.
New or progressive weakness, changes in coordination, or balance problems raise additional concern, especially when they affect daily activities such as climbing stairs, rising from a chair, or maintaining steady footing. These symptoms may indicate involvement of motor nerves or the spinal cord and deserve timely assessment.
Evaluation is also appropriate when nerve pain does not respond to over-the-counter medications, basic home care, or standard physical therapy. In these cases, advanced imaging and targeted diagnostics can help identify the underlying cause and guide more effective treatment. Early specialist involvement often improves outcomes by addressing nerve dysfunction before it becomes chronic or disabling.
Why Choose Peloza Spine in Chesterfield, MO
Peloza Spine stands out in Chesterfield, MO for patients seeking expert care for complex, nerve-related spine pain.
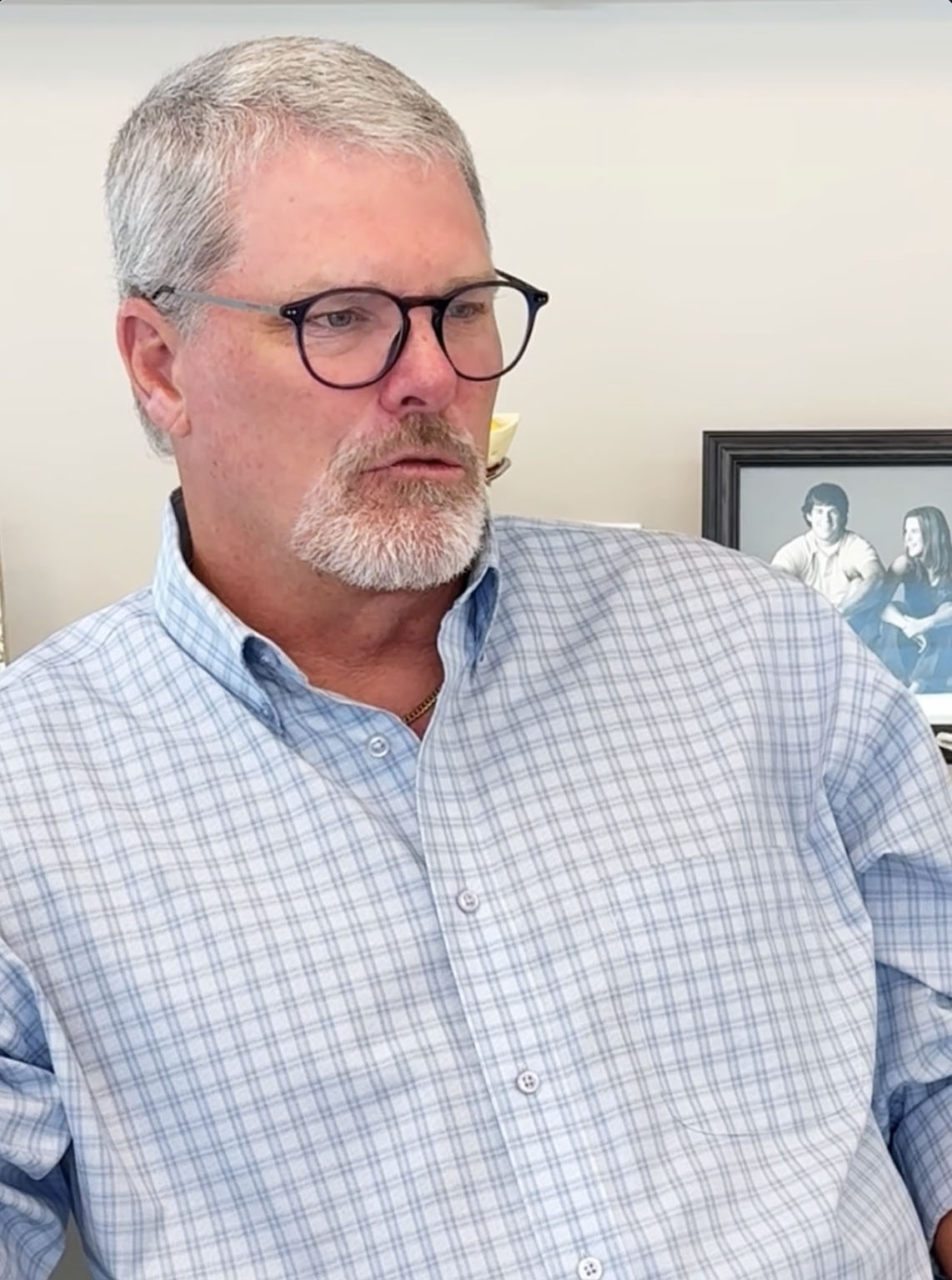
- Expertise: Dr. John Peloza is a board-certified orthopedic spine surgeon with more than 30 years of experience, recognized nationally and internationally for his work in motion-preserving spine surgery, artificial disc replacement, endoscopic surgery, and regenerative techniques.
- Precision: Peloza Spine uses sophisticated imaging, navigation, and data-driven planning to pinpoint the exact source of nerve pain and tailor both non-surgical and surgical treatments to each patient’s anatomy and goals.
- Compassionate Care: Patients consistently describe Dr. Peloza as thorough, communicative, and deeply focused on quality of life, supported by a professional team that coordinates in-person and telehealth visits and helps guide patients through every step of care.
Located in Chesterfield, Missouri, and serving the greater St. Louis region, Peloza Spine also welcomes patients from across the country, offering concierge support for travel, lodging, and scheduling so out-of-town patients can access world-class care with less stress.


Take the First Step
Toward Nerve
Pain Relief
Persistent nerve pain can limit sleep, mobility, and daily life. When symptoms continue, a precise diagnosis is the first step toward meaningful relief. A consultation with Dr. John Peloza in Chesterfield focuses on identifying the underlying cause of neuropathic pain and determining which treatments are most likely to help. Peloza Spine offers in-person visits and secure virtual consultations, with coordinated support for patients traveling from outside the region. If nerve pain is affecting your quality of life, a specialist evaluation with Dr. Peloza can provide clear direction and a personalized plan forward.
Frequently Asked Questions
How do I know if my leg pain is from claudication or something else?
If your leg pain eases when you sit or lean forward but worsens when you walk or stand, that pattern suggests neurogenic claudication rather than a vascular cause.
Will I need surgery for claudication?
Many patients respond well to conservative treatments. Dr. Peloza recommends surgery only when non-surgical options haven’t provided adequate relief and nerve compression is significantly affecting your quality of life.
How long is recovery after minimally invasive surgery?
Recovery varies by procedure, but minimally invasive techniques generally allow for faster healing—often weeks rather than months. Dr. Peloza will provide a personalized recovery timeline based on your specific treatment.
Can claudication get worse over time?
Yes. Without treatment, spinal stenosis and nerve compression can gradually worsen, leading to increased pain, numbness, or weakness and further limiting how far you can walk. The good news is that early evaluation and treatment often stop progression, relieve symptoms, and help preserve your mobility for the long term.
FROM OUR PATIENTS
“Dr. Peloza is outstanding. His bedside manner is bar none-he's compassionate, patient, and genuinely cares about his patients. He is incredibly smart, explains things in a way that makes you feel confident and informed, and never rushes you. I wouldn't trust anyone else with my spine issues and feel very lucky to have found him.”
- Cathy C.,
“I had disabling back pain interfering with my work, my sleep, and my leisure. After consulting several excellent physicians in Dallas who all recommended complicated fusion surgery I traveled to see Dr. Peloza and had surgery without a fusion and its downrange complications. 1 month later I am pain free and once again active in all daily activities. His staff is amazing and they coordinate all aspects of your care and do a great job on Tele care as well. Dr. Peloza cares about his patient's quality of life and their perception of care. There is none better when it comes to bedside manner, patient communication, expertise in the field, and access to care. Don’t want to be another 'Postlaminectomy syndrome on chronic pain meds' - Then this is the place to trust for your care!”
- AS,
“Dr. Peloza and his staff were incredible to work with from the beginning of my diagnosis to the surgery and the aftercare. Would highly recommend him!!”
- Michael J.,
“I’m extremely pleased, I feel honored to recommend Dr. Peloza to everyone. I can actually say he saved me and changed my life. I now feel like I have a reason to get up and enjoy the beautiful day that God blessed me with.”
- Deb J.,
“I absolutely think this man is an amazing doctor! He replaced 4 discs in my C-spine and he is doing my lumbar spine very soon! I HIGHLY HIGHLY recommend him! I am so grateful for everything!”
- Cathy W.,
“Dr. Peloza is an extremely gifted surgeon and practitioner. I have recommended him to anyone who will listen to how having a disc replacement has changed my life!”
- Jacque C.,
“Dr. Peloza has been phenomenal from the first day I saw him! His extended tests helped to get a proper diagnosis, as well as he has been quick to come up with a treatment plan for me. His staff are professional, friendly, and quick to offer help. One of the best!”
- Kelly M.,
CASE HIGHLIGHTS
Discover breakthrough treatments and
remarkable patient recoveries.