Claudication Treatment
Find relief from leg pain and numbness caused by spinal stenosis right here in Chesterfield, just outside St. Louis.

ADVANCED TECHNOLOGY MEETS
SURGICAL EXPERTISE
What Is Claudication?
Claudication is leg pain, numbness, or weakness that occurs when you walk or stand for extended periods. Many people describe it as heaviness, cramping, or tingling that makes it difficult to stay active. The good news? Resting or bending forward typically brings relief—and that’s an important clue about what’s causing your symptoms.
There are two main types of claudication. Vascular claudication results from poor blood flow to the legs, while neurogenic claudication stems from nerve compression in the lower spine. Dr. Peloza specializes in treating neurogenic claudication, helping patients overcome the spinal issues that trigger leg pain and restore their ability to walk comfortably.
REDEFINING WHAT RECOVERY CAN LOOK LIKE
Common Causes of
Claudication
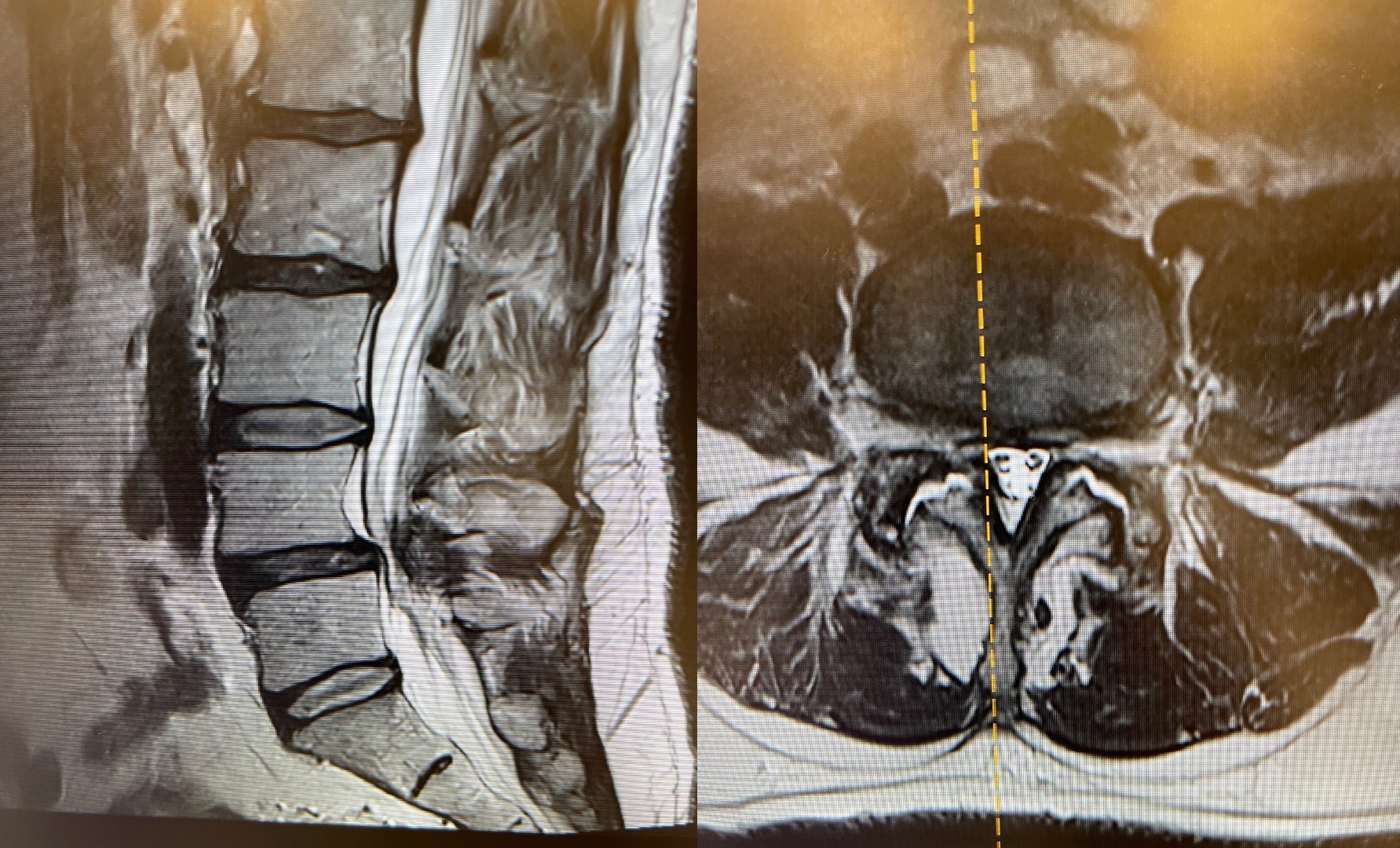
Lumbar Spinal Stenosis
The most common cause of neurogenic claudication is lumbar spinal stenosis—age-related narrowing of the spinal canal that puts pressure on nerves traveling to your legs. As we age, changes in the spine such as thickened ligaments, bone spurs, and bulging discs can gradually reduce the space available for nerves. When you stand or walk, this compression intensifies, triggering the characteristic leg symptoms of claudication.
Degenerative Disc Disease
When spinal discs lose height and cushioning over time, the space between vertebrae narrows. This can lead to nerve compression and claudication symptoms, particularly during activities that load the spine.
Facet Joint Hypertrophy & Arthritis
As facet joints undergo wear and tear over time, they can become enlarged and arthritic. This thickening, combined with enlarged ligaments and bone spurs, further narrows the spinal canal and adds pressure to nerve roots. Facet joint arthropathy is one of the primary culprits in lumbar spinal stenosis, particularly affecting the superior articular facets.
Herniated or Bulging Discs
A herniated or bulging disc can press directly on spinal nerves, causing pain that radiates down one or both legs. While these conditions often cause acute symptoms, chronic compression from either type can contribute to claudication over time, particularly when combined with spinal stenosis.



Recognizing the Symptoms of Claudication
If you notice leg pain or weakness that begins when you walk but eases when you sit or lean forward, you may be experiencing claudication.
Neurogenic claudication follows a distinctive pattern: symptoms worsen with activity and improve with rest. You may feel pain, numbness, tingling, or weakness that starts after walking a certain distance or standing for a period of time. Many patients find relief when they sit down or bend forward—such as when pushing a shopping cart—because that position opens space in the spinal canal and reduces nerve pressure.
Unlike vascular claudication, which causes calf pain from reduced blood flow, neurogenic claudication can affect multiple areas of both legs and often produces a heavier, more diffuse discomfort. Recognizing these differences can help you and your physician determine whether spinal nerve compression is the true source of your symptoms.
How Dr. Peloza
Diagnoses Claudication
At Peloza Spine, every diagnosis begins with attentive listening. Dr. Peloza takes time to understand your symptoms, medical history, and how leg pain or weakness affects your daily life. This patient-centered approach ensures that every detail from when symptoms appear to how far you can walk and what positions bring relief guides the next steps in evaluation.
A focused physical and neurological exam follows, assessing strength, reflexes, sensation, balance, and walking mechanics. Dr. Peloza also examines spinal flexibility and alignment to pinpoint areas where nerve compression may occur. These findings often reveal patterns that distinguish neurogenic claudication from other causes of leg pain.
Advanced imaging provides a precise view of the underlying problem. MRI, CT, and X-ray studies together show how much space the spinal nerves have and where that space has narrowed. When needed, additional tests such as electromyography (EMG) or nerve conduction studies help measure nerve function directly. This thorough, evidence-based process allows Dr. Peloza to identify the exact source of your symptoms and design a treatment plan tailored to your needs.


Non-Surgical
Treatment Options
Most patients with neurogenic claudication find meaningful relief without surgery. Dr. Peloza tailors each non-surgical plan to the individual, combining therapies that ease nerve pressure, reduce inflammation, and improve spinal stability.
Physical therapy focuses on restoring flexibility and strengthening the muscles that support your spine, helping you move more comfortably and with better balance. Activity modification teaches you how to position your body to relieve pressure on spinal nerves, such as leaning forward slightly or using support while walking. Medications can reduce inflammation and calm irritated nerves, while targeted injections such as epidural steroids or selective nerve root blocks offer focused pain relief when symptoms persist.
Equally important are lifestyle adjustments that protect long-term spinal health. Weight management, posture correction, and smoking cessation all help reduce stress on spinal structures and improve circulation to the nerves. Together, these measures often restore function and comfort, allowing many patients to walk farther and live more actively without surgery.
Minimally Invasive & Advanced Procedures
When conservative care no longer provides adequate relief, Dr. Peloza offers advanced procedures that target nerve compression with minimal disruption to surrounding tissues. His approach focuses on precision, shorter recovery times, and preserving spinal motion whenever possible.
- Laminectomy or Laminotomy: Surgical decompression procedures that widen the spinal canal, creating more space for nerves and reducing pain from spinal stenosis.
- Artificial Disc Replacement: Replaces a collapsed or damaged disc to restore disc height, relieve nerve compression, and maintain natural spinal movement.
- Hybrid Solutions: Combines advanced techniques to stabilize the spine while protecting motion at adjacent levels and preventing future degeneration.
These procedures reflect Dr. Peloza’s commitment to modern, motion-preserving spine care. Dr. Peloza is committed to helping patients regain mobility, reduce pain, and return to the active lives they love with as little downtime as possible.


When to See a
Spine Specialist
for Claudication
Knowing when to seek expert care can make a crucial difference in outcomes. Claudication often begins subtly, but if symptoms persist or worsen, professional evaluation becomes essential to prevent long-term nerve damage and restore mobility. You should see a spine specialist if you experience:
- Pain or weakness that limits how far you can walk or prevents you from standing comfortably.
- Persistent numbness or tingling in your legs that does not improve with rest or physical therapy.
- Progressive loss of balance or coordination, making it harder to walk steadily or perform routine activities.
- A noticeable decline in quality of life caused by fear or avoidance of walking and standing due to leg pain.
If these signs sound familiar, Dr. Peloza can determine whether spinal nerve compression is the cause and design a personalized treatment plan to help you move comfortably and confidently again.
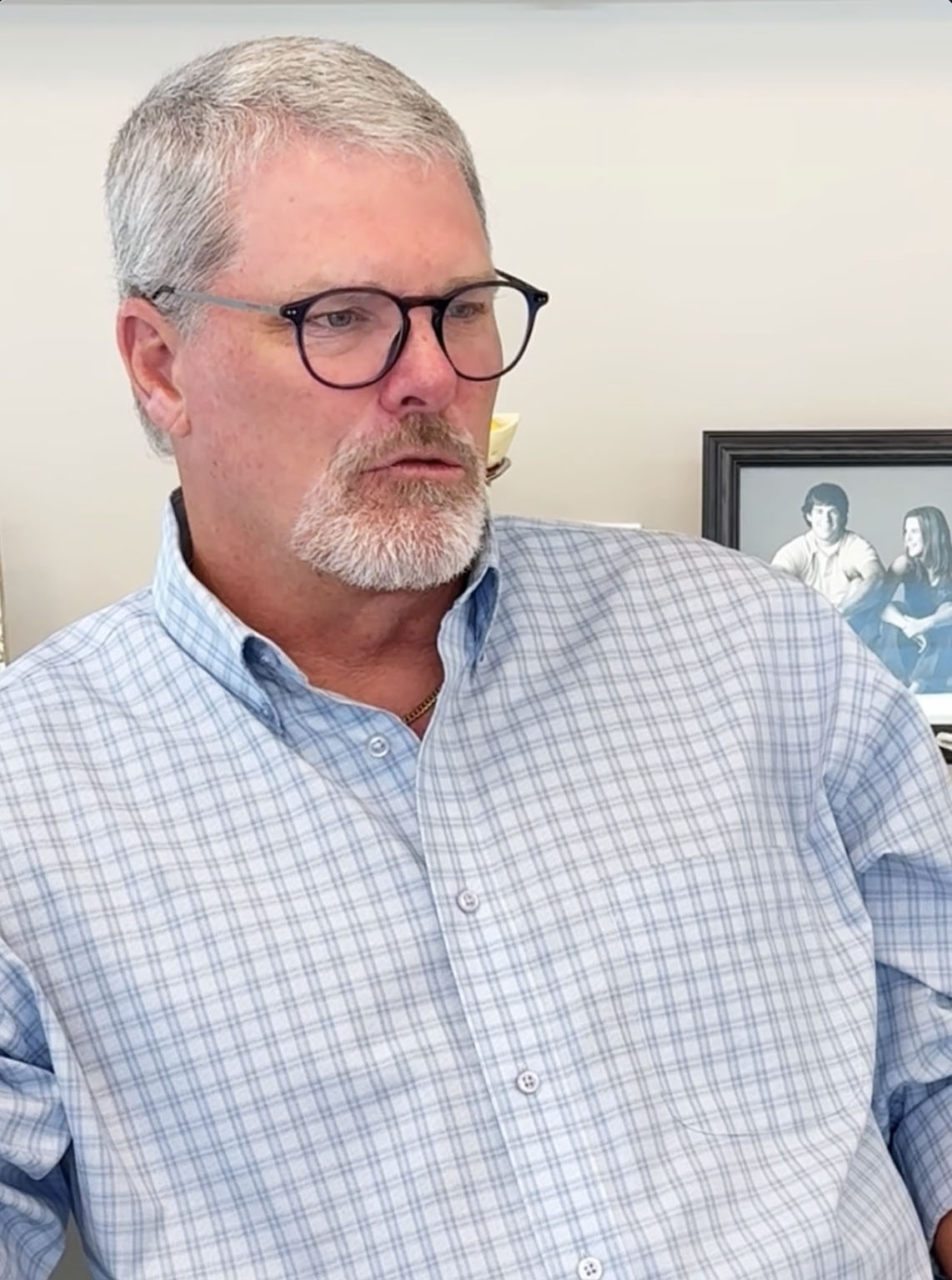
Why Choose Peloza Spine in Chesterfield, MO
As a nationally recognized spine surgeon with more than 30 years of experience, Dr. John Peloza brings unmatched expertise to every patient consultation. A leader in spine surgery research and innovation, he has helped advance motion-preserving and minimally invasive techniques that deliver relief while protecting long-term spinal health.
Dr. Peloza’s practice philosophy centers on truly personalized care. Rather than taking a one-size-fits-all approach, he tailors each treatment plan to your specific symptoms, goals, and lifestyle. He takes time to explain your diagnosis clearly and discusses every available option, from conservative therapies to advanced surgical procedures, so you can make informed decisions with confidence.
Patients benefit from Dr. Peloza’s commitment to using minimally invasive methods whenever possible—an approach that means smaller incisions, less tissue disruption, reduced pain, and faster recovery. His extensive experience treating complex spinal disorders ensures that every patient receives care grounded in both clinical expertise and the latest scientific evidence.

Take the First Step
Toward Relief
If leg pain or weakness limits your ability to stay active, now is the time to take the first step toward lasting relief. Schedule a consultation with Dr. John Peloza to uncover the true cause of your symptoms and explore treatment options tailored to your needs. Peloza Spine welcomes both local and out-of-town patients, offering virtual consultations for convenience and coordinated support for those traveling to the practice. Most major insurance plans are accepted, and our Chesterfield office provides easy access for patients throughout the St. Louis area. Relief and restored mobility begin with an expert diagnosis—schedule your consultation today.
Frequently Asked Questions
How do I know if my leg pain is from claudication or something else?
If your leg pain eases when you sit or lean forward but worsens when you walk or stand, that pattern suggests neurogenic claudication rather than a vascular cause.
Will I need surgery for claudication?
Many patients respond well to conservative treatments. Dr. Peloza recommends surgery only when non-surgical options haven’t provided adequate relief and nerve compression is significantly affecting your quality of life.
How long is recovery after minimally invasive surgery?
Recovery varies by procedure, but minimally invasive techniques generally allow for faster healing—often weeks rather than months. Dr. Peloza will provide a personalized recovery timeline based on your specific treatment.
Can claudication get worse over time?
Yes. Without treatment, spinal stenosis and nerve compression can gradually worsen, leading to increased pain, numbness, or weakness and further limiting how far you can walk. The good news is that early evaluation and treatment often stop progression, relieve symptoms, and help preserve your mobility for the long term.
FROM OUR PATIENTS
“Dr. Peloza is outstanding. His bedside manner is bar none-he's compassionate, patient, and genuinely cares about his patients. He is incredibly smart, explains things in a way that makes you feel confident and informed, and never rushes you. I wouldn't trust anyone else with my spine issues and feel very lucky to have found him.”
- Cathy C.,
“I had disabling back pain interfering with my work, my sleep, and my leisure. After consulting several excellent physicians in Dallas who all recommended complicated fusion surgery I traveled to see Dr. Peloza and had surgery without a fusion and its downrange complications. 1 month later I am pain free and once again active in all daily activities. His staff is amazing and they coordinate all aspects of your care and do a great job on Tele care as well. Dr. Peloza cares about his patient's quality of life and their perception of care. There is none better when it comes to bedside manner, patient communication, expertise in the field, and access to care. Don’t want to be another 'Postlaminectomy syndrome on chronic pain meds' - Then this is the place to trust for your care!”
- AS,
“Dr. Peloza and his staff were incredible to work with from the beginning of my diagnosis to the surgery and the aftercare. Would highly recommend him!!”
- Michael J.,
“I’m extremely pleased, I feel honored to recommend Dr. Peloza to everyone. I can actually say he saved me and changed my life. I now feel like I have a reason to get up and enjoy the beautiful day that God blessed me with.”
- Deb J.,
“I absolutely think this man is an amazing doctor! He replaced 4 discs in my C-spine and he is doing my lumbar spine very soon! I HIGHLY HIGHLY recommend him! I am so grateful for everything!”
- Cathy W.,
“Dr. Peloza is an extremely gifted surgeon and practitioner. I have recommended him to anyone who will listen to how having a disc replacement has changed my life!”
- Jacque C.,
“Dr. Peloza has been phenomenal from the first day I saw him! His extended tests helped to get a proper diagnosis, as well as he has been quick to come up with a treatment plan for me. His staff are professional, friendly, and quick to offer help. One of the best!”
- Kelly M.,
CASE HIGHLIGHTS
Discover breakthrough treatments and
remarkable patient recoveries.